Short Sleep and Weight Gain

We’ve all felt how short sleep can impair our ability to think, feel, and perform our best. A night of bad sleep happens from time to time – lethargy, fogginess, and/or irritability are all but impossible to shake. Fortunately, with a good night of sleep we’re usually as good as new.
In contrast, chronic shortened sleep presents more insidious issues. One out of every three adults in the US gets less than the recommended 7 hours per night.[1] Further, per the National Sleep Foundation, 35% of polled individuals report sleep quality as “poor” or “only fair”.[2]
Drivers of Short Sleep and Weight/Fat Gain
Data demonstrates a linkage between shortened sleep and increased risk of developing obesity, diabetes, heart disease, stroke, and mental distress. Decreased sleep duration and quality is associated with increased body weight and body fat. Epidemiological evidence supports the role of inadequate sleep contributing to the high prevalence of obesity (in children and adults).
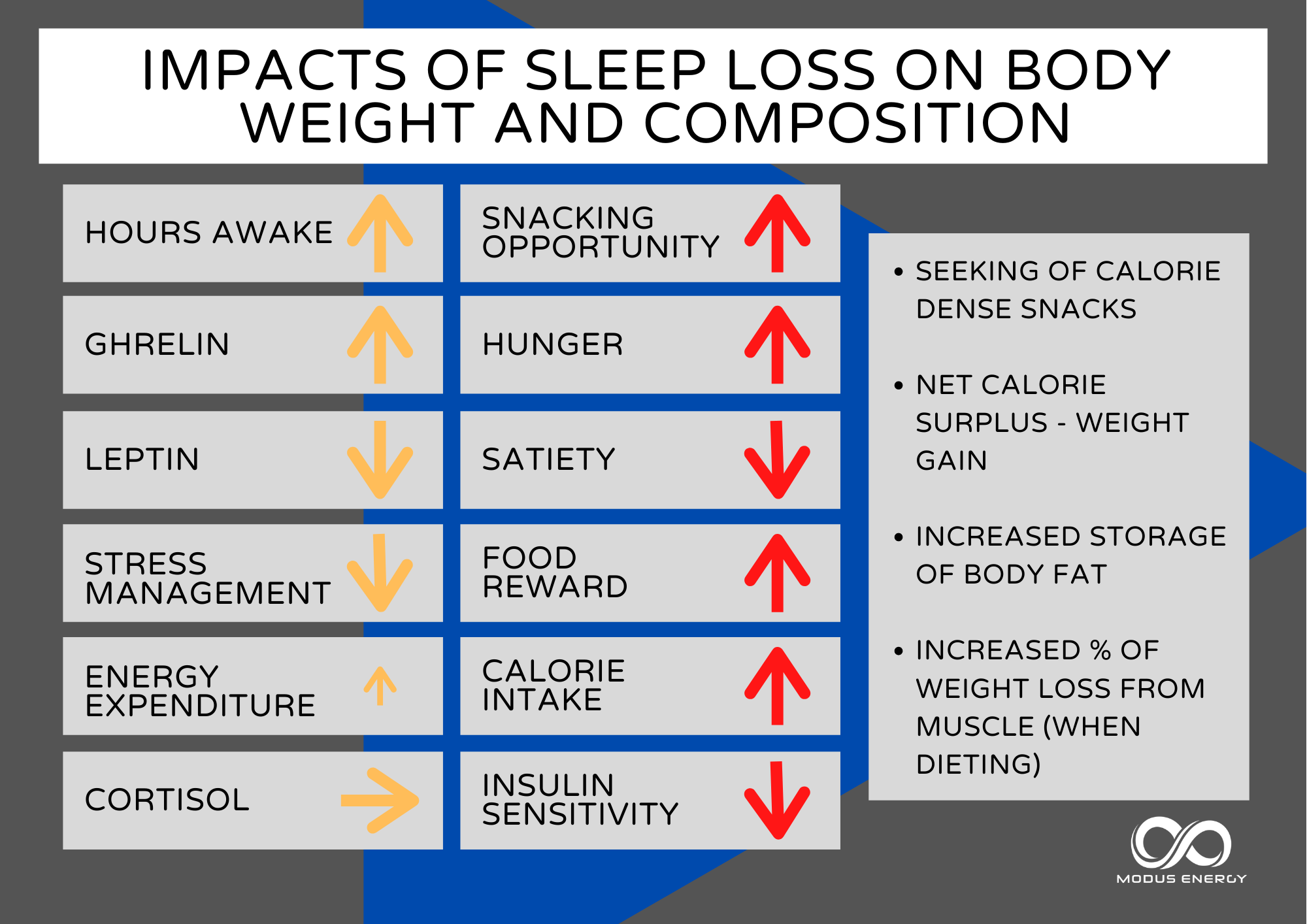
The drivers behind short sleep and weight gain, increased fat mass, and potential loss of muscle/lean mass are highly interconnected.

1. Increased hunger and reduced satiety
Sleep, food, activity, and stress directs our body to release or throttle back certain hormones. In turn, these hormonal signals can influence our behaviors. Leptin and ghrelin are two hormones that contribute to our regulation of food intake. Leptin aka the “satiety hormone” is released by our fat cells and communicates our energy status to the brain. Levels increase as we eat and become full – telling the central command center “all good – we have energy”. Generally, leptin levels are lowest in the morning and build throughout the day as we consume food. They peak into the evening. Lower leptin levels are associated with decreased satiety from food and drive to increase energy intake. Ghrelin, a.k.a. the “hunger hormone”, is released by stomach cells to stimulate our appetite. Levels rise when are hungry, and fall when we are full.
Depending on the nature of sleep debt, leptin levels may fall and ghrelin levels may rise. Our bodies are signaling our brain for extra calories, and those calories are likely coming from additional fat and/or carbohydrates.
A randomized crossover study examined appetite regulation after 2 nights of 4 h in bed and after 2 nights of 10 h in bed. Leptin levels decreased by 18% after the short nights relative to the long nights in bed. Ghrelin increased by 28% increase after the short nights relative to the long nights. Participants filled out questionnaires on hunger and appetite, indicating a 24% increase in hunger and a 23% increase in global appetite after the 4-hour nights versus the 10-hour nights. Appetite for high carbohydrate nutrients was the most affected with a 32% increase.[3]
Another study demonstrated a correlation between shortened sleep and increased energy intake, and particularly fat intake.[4] In a group of middle-aged men and women, the study controlled dietary intake for 3 days, followed by 2 days of free eating during 5 nights of 4 h time in bed compared with 9 h time in bed. Energy intake increased by about 300 kcal/day in the 4h sleep condition, with notable increase in dietary fat intake, suggesting a preference toward high fat foods under conditions of sleep deprivation.
Catch-up sleep does not appear to be an effective strategy. We don’t re-set our calorie intake back to baseline levels even if we can get multiple nights of extended sleep.
In an 18 day laboratory study, participants were placed in a varying sleep-restricted/recovery group (varying numbers of sleep restricted days (4 h of time in bed) and recovery days (12 h time in bed) or a control group (allowed 10 h time in bed every night). Regardless of the ratio of sleep restricted to recovery days, all participants that had some days of sleep restriction had increased daily intake, on average, in excess of 500 kcal/day versus the control group.[5] In short, weekend catch up sleep is unlikely to lead to reduced calorie intake if intake levels were elevated during short sleep periods.
2. More hours awake + access to tasty food + increased reward response = increased calorie intake (likely from extra snacking)
Although it may seem obvious, reduced sleep means that there are more waking hours available to eat.
One study conducted over 14 days compared a group of men and women who either had 8.5 or 5.5 h time in bed, with both groups able to freely eat meals and snack foods as they desired. During the 5.5 h condition, participants consumed significantly more snacks after dinner (with no change in meal intake between groups), and chose snacks were higher in carbohydrate content.[6]
Considering some studies report no significant changes in ghrelin and leptin levels with reduced sleep, hedonic factors may contribute to increased weight gain and adiposity. The impact of short sleep duration on stress response and reward-seeking behavior can be powerful, and stronger in certain individuals than in others.
A key region in the brain frontal cortex plays a strong role in our perception of representations of food. Higher activation of this brain region has been found in obese compared with normal-weight test subjects when anticipating food[7] indicating that the reward we get from food is enhanced in obesity.
A similar response is found in normal-weight individuals after one night of total sleep deprivation, indicating prolonged wakefulness leads to greater reward response in anticipation of food. Sleep deprivation is also associated with lower scores in stress management skills which may tie directly to increased consumption of palatable foods. Specifically, reduced impulse control and difficulty to delay gratification.
3. Energy mismatch problem: increased calorie intake is higher than additional energy expenditure in shortened sleep
Chronic partial sleep deprivation leads to feelings of fatigue and slowness,[8] so you may expect that total daily energy expenditure (TDEE) decreases with less sleep. However, TDEE is slightly higher with shortened sleep.
Findings show that, compared to 8h per night baseline sleep, energy expenditure increased by ∼7% during the first 24h of sleep deprivation, and then decreased by 5% upon resumption of normal sleep. During the night, energy expenditure increased by ∼32% during sleep deprivation, and then decreased approximately 4% during recovery sleep.[9]
The reality is that although we are expending more energy by sleeping less, this increase is small. Missing one complete night of sleep provides an additional “burn” of about 130 Calories, and this would be far less for shortened sleep versus total sleep loss. If we are snacking an additional 300-500 Calories in excess due to prolonged wakefulness coupled with only needing minimal additional calories, it’s easy to see how the calorie surplus adds up day after day resulting in fat accrual.
4. Higher % weight gain from fat (or loss of less fat when dieting)
Increased levels of evening cortisol and reduced growth hormone secretion may prompt the body to store more fat at the expense of muscle and other tissues for energy during shortened sleep.
Cortisol, our “stress response” hormone is controlled by circadian rhythmicity. The 24-hour profile of cortisol is characterized by an early morning maximum, declining levels throughout the daytime, a period of minimal levels in the evening and first part of the night, and an sharp circadian rise in later part of the night. With shortened sleep, the body maintains higher levels of cortisol later in the day, at a point where we should we winding down and readying ourselves for sleep. Even two nights of sleep restriction (4 h compared with 10 h in bed) in normal or moderately overweight men was associated with a 21% evening cortisol elevation. Heightened cortisol makes our body tissues less sensitive to insulin[10] prompting the body to store more fat and utilize other fuel sources (muscle!) for energy. It is established that those on a diet will lose less fat and more muscle as a percent of total weight lost when sleep is restricted. [11]
I hope this summary provided you some insights on the importance of sleep! In addition to nutrition, sleep is an area we examine closely in 1:1 coaching. There are a number of tactical tools we implement to ensure you are maximizing your results. We endeavor to give you as much energy as possible and mitigate the risk of fat gain and muscle loss.
A few ideas to help with sleep:
– Enable “night mode” on your phone to reduce blue light exposure. Set the timing from sunset to sunrise. If you are watching TV or on a laptop, consider wearing blue blocker glasses.
– Cease consuming food ~2h before bed (unless you have circumstances that require later eating).
– Solidify a nighttime calming ritual, starting about 1h before bed. For example – electronics off, brush teeth, breathing exercises, reading a book.
[1] https://www.cdc.gov/sleep/data_statistics.html
[2] Knutson, K.L; Phelan, J.; et al., The National Sleep Foundation’s Sleep Health Index, Sleep Health, 3(4), 234, 2017.
[3] Spiegel K., Sleep curtailment in healthy young men is associated with decreased leptin levels, elevated ghrelin levels and increased hunger and appetite. Ann Intern Med. 141, 846–850, 2004.
[4] St-Onge M-P, Roberts AL, Chen J, et al., Short sleep duration increases energy intakes but does not change energy expenditure in normal weight individuals. Am J Clin Nutr. 94(2), 410-416, 2011.
[5] Spaeth, A.M.; Goel, N.; et al., Caloric and Macronutrient Intake and Meal Timing Responses to Repeated Sleep Restriction Exposures Separated by Varying Intervening Recovery Nights in Healthy Adults, Nutrients, 12, 2694, 2020.
[6] Nedeltcheva A.V.; Kilkus, J.M.; et al., Sleep curtailment is accompanied by increased intake of calories from snacks. Am J Clin Nutr., 89(1), 126-133, 2009.
[7] Martin L.E.; Holsen, L.M.; et al., Neural mechanisms associated with food motivation in obese and healthy weight adults. Obesity (Silver Spring), 18, 254 –260, 2010.
[8] Dinges D.F.; Pack, F.; et al., Cumulative sleepiness, mood disturbance, and psychomotor vigilance performance decrements during a week of sleep restricted to 4–5 hours per night. Sleep, 20, 267–77, 1997.
[9] Jung, C.M.; Melanson, E.L.; et al., Energy expenditure during sleep, sleep deprivation and sleep following sleep deprivation in adult humans., J Physiol.,589 (Pt 1), 235-244, 2011.
[10] Donga, E.; van Dijk, M.; et al., A single night of partial sleep deprivation induces insulin resistance in multiple metabolic pathways in healthy subjects., J Clin Endocrinol Metab., 95(6), 2963-2968, 2010.
[11] Nedeltcheva, A.V.; Kilkus, JM.; et al., Insufficient sleep undermines dietary efforts to reduce adiposity, Ann Intern Med., 153(7), 435–441, 2010.



